How Aetna Calculates Out of Network Claim Amounts?
Most health plans pay for out-of-network care based on what's called the "reasonable," "usual and customary," or "prevailing" charge. This article will explain how Aetna out-of-network claim works.

Some health plans pay for services from providers who are not in the plan’s network based on what is called the “reasonable,” “usual and customary,” or “prevailing” charge. Aetna gets this information from a company that collects and analyzes data on charges for services provided by doctors in different areas. It then creates a database that shows what the typical doctor charges for each procedure. When a member uses a provider outside the network, the health plan pays 70 percent of that prevailing charge. The doctor then bills the member for the remaining 30 percent.
Providers send Ingenix copies of claims for services they receive from members, along with the date and place of the service and the provider’s charge. Ingenix then combines this information into databases that show how much providers charge for each service in different zip codes. When a member uses an out-of-network doctor, Aetna pays 70 percent of the plan’s recognized charge (also known as the prevailing charge). The remaining 30 percent is the responsibility of the member. These charges do not count toward the member’s deductible or out-of-pocket limit.
Can You Submit Claims Electronically to Aetna?
You can submit claims electronically to Aetna by using the online provider portal. This allows you to view your explanation of benefits (EOB) and check your claim status within 45 days after submission. The online provider portal also allows you to upload invoices for payment processing. However, you must submit your invoice to Aetna within 60 days of the date of service. But for some plans, care from out-of-network doctors and hospitals is covered as well. You may have to pay more for out-of-network care, though.
Many Aetna plans only pay for care that’s received from in-network providers. However, some plans cover some level of care provided by non-network providers. However, out-of-network benefits are subject to deductibles and coinsurance. Typically, out-of-network care costs more than in-network care because the provider does not have a contract with your plan.
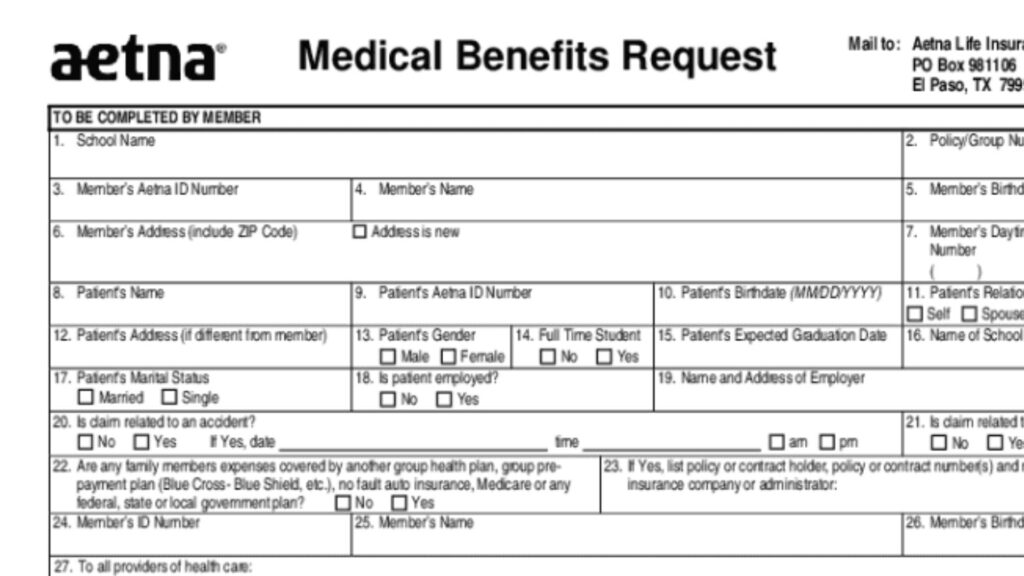
Filling out the Aetna claim form is a complex process and should be done carefully to ensure accurate information. Incorrect or incomplete information can delay processing and result in the forfeiture of funds. Double-check your form before submitting it, and keep a copy for your records. Providing a copy of the itemized bill and receipts will help speed up the process.





